|
Service Integration and ‘person-centered care’ – two phrases that are so easy to say and yet very challenging to genuinely put into practice. However, service integration is essential and has been ever since I first became a social worker in 1980. The field I worked in was Child Protection – then, as now, we needed to form a circle of care around the child and his/her family to support the child and the adult/s to care for their child/ren. Relationships were key – our relationships with other agencies and our relationships with the family members. Without email or texts, we set up meetings to ‘co-ordinate’ our services.
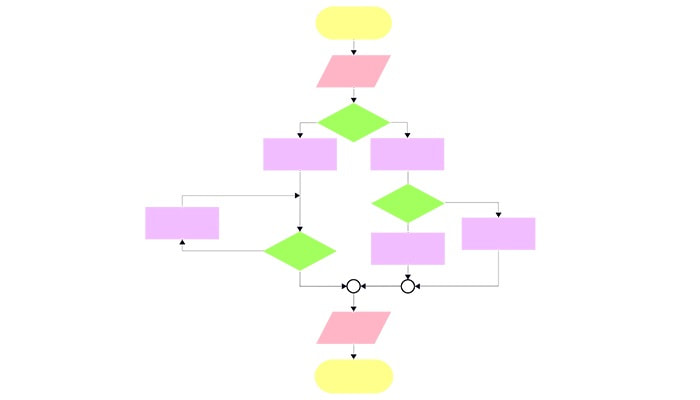
Moving rapidly to today where the expectation is that services are co-designed, co-ordinated, integrated and that we have the ‘person’ at the centre of all care – in other words, the person receiving any care, is in charge of that care and making their own choices and decisions. Many health and human services websites now reflect ‘person-centered care’. How do we ensure that ‘person-centered care’ is really happening? I would argue that any organisation involved in caring for a person needs to share similar values, similar attitudes and similar definitions around what is ‘person-centered care’ and be experienced in partnering – both at the inter-agency system level and at the service provision level. Furthermore, the way the system of care is funded will influence the capacity of services to practice in a person-centered manner. If organisations continually compete for funding at senior levels, this will likely be reflected in the network of services and their frontline staff. For those providing the services and care, I believe that a flow chart of who will do what when is essential in ensuring workers understand in principle their role and responsibilities in caring for a person. This needs to be flexible and adaptable to the individual needs as expressed by the person. When workers are clear on their role, the care they will provide and how they will communicate professionally with other services, this hopefully leads to the person better understanding their care and able to make choices that best meet their needs. A flow chart sounds elemental, however, the very visual nature of developing the chart is extremely helpful to those who need to work together. Hosting a workshop to map out who does what, how it is recorded, and, what the lines of communication are, is both a recording activity (map of pathways with the person at the centre) and a problem-solving one. As the care flow chart is drawn and redrawn, workshop participants genuinely talk about how they work together and across their services. There are usually ‘aha’ moments as one professional describes what they do and understands how this needs to dovetail in with another activity. In my experience, the most efficient initial workshop recording is done using a sticky wall – this allows for any steps to be easily moved or re-written as they are on separate pieces of paper that stick to the wall. The question at every step of the journey is ‘how does this serve the person we are here to provide care with and for?' The workshop needs to include all potential agencies in the service network; all attending with the same purpose to continually improve the way in which care is provided to the person. Comments are closed.
|
AuthorJill Nicholson Archives
August 2023
Categories
All
|